We are living through an uncomfortable period in the practice of medicine.
The dialogue between patient and physician is critically underserved, both in terms of tools for patients and physicians, and also in terms of the data context where that conversation takes place. This is unfortunate, because those are the moments of human to human care. Whether it’s a clinic visit, a lab test, a counseling or physical therapy session, the patient / provider meeting is when the full breadth of the caregiver’s experience and training can be brought to bear. At these moments, the subtle observations and pattern recognition that constitute diagnostic expertise come into play. These are are also the times when the nuance and detail of the patient’s lived experience can be shared to influence the course of diagnosis and treatment.
Population health turns into personal medicine at the bedside.
That conversation between patient and physician ought to be a first class citizen in terms of tool development, but it is not. It is within our reach to build a clinical care environment that retains high standards of data integrity and privacy while also focusing on empowering the human beings in the room rather the interests outside the door.
Due to the misaligned incentives that I’ve written about previously, the development of tools to support a data-rich conversation between patient and physician has generally taken a back-seat to software for billing, regulatory compliance, and mitigating risks to the care system. Recently, we have begun to instrument the clinic to support data gathering for research purposes. While this is a great idea on the face of it, it can have the unintended effect of leaving still less time for that critical conversation. Unless we can close the loop and bring the benefit of that instrumentation back to either physician or patient, it will be felt as friction, yet another loss.
I believe that we can have our data and do research on it too – and also that the clinical interaction is vastly more important than research use of the data we might gather along the way.
Research at no benefit to the participant
On the topic of research.
I’ve participated in a number of clinical research projects, mostly around genetics and genomics. The usual routine is to sit in a plastic chair and fill out a piece of paper using a pen tied to a clipboard. Some projects let me do the (still manual) data entry using a tablet. I used to gripe to the staff that this is a terrible, terrible way to gather data, but these days I just let them do their job and then blog or tweet about it later. The moment of truth comes with a needle stick, a swab, or a collection cup. Sometimes there are juice and cookies. Usually not.
Later, some anonymous lab will re-measure values that I’ve likely already got on my laptop. The math is churned for a few months, and perhaps somebody publishes. I usually won’t find out. I’ve stopped asking about that, because I’m bored with people who use HIPAA as an incantation to ward off further questions.
There are notable exceptions to this pattern of research’s stony indifference to the well being of the participants. The Coriell Personalized Medicine Collaborative stays in touch, nearly a decade after I spat in a tube for them. I get regular emails sharing the research results derived from my data. They also provide a crufty-but-effective web interface to allow me see curated and IRB approved subsets of my results along with risk scores and background reading. For all the well-deserved flak we give (and should continue to give) 23andme for selling our data to the highest pharmaceutical bidder without asking first – they too give me useful and regular value.
All of Us is saying the right words about citizen researchers and “partners rather than subjects,” but the proof will be in the pudding. Their involvement with the likes of Google leaves me a bit cold.
In nearly two decades of energetically engaged participation, I have yet to encounter even one research project that offered to close the loop on the data they collected by making it available to my physician in the context of my clinical care. Nearly two decades after we completed the Human Genome Project, this basic courtesy to research participants is still not on the menu.
We are left to fend for ourselves, to separate the useful offerings from the snake oil in the direct to consumer marketplace.
Personal Data
I’ve written, more than once, about my ongoing attempts to get out in front of the curve of personalized / precision medicine. I can see where we’re going, and I want to live there as soon as possible. Early 21st century medicine is, by and large, reactive. Nobody wants to hear, “I wish we had caught this earlier,” but that’s what you get when the protocol is to wait for visible symptoms before testing for disease. Risk officers exacerbate this by steering physicians away from data, citing the risk of incidental findings and HIPAA violations.
I’m still irked about the physician who tried to refuse to screen me for the colorectal cancer that killed my grandfather, despite genetic and symptomatic evidence that indicated that it might be worth an extra look.
In the future, patients will have conversations about their care in the context of a well structured repository of personal data. That data will come from multiple sources, most of them nonclinical. Our data will be available, with appropriate localization for education and language, directly to the patient. We will be able to share it with our in-home caregivers and with a care team that includes both physicians and other health and wellness professionals.
In the future, nobody will ask for my previous doctor’s FAX number.
Put another way, our physicians should have the same data-driven advantages that we already see in retail sales, in entertainment, and in finance. Our doctors should have the kind of integrated data that data monopolies like Google, Amazon, and Apple already use to influence everything from our buying to our voting.
Of course, that will require changes to – without exaggeration – nearly every aspect of the clinical data environment. We should start now if we want to see it in our lifetimes.
Mercury Retrograde
A company named Arivale has been a partner in my personal data journey for the last year. Through them, I could get clinical-grade laboratory bloodwork every six months. The Arivale dashboard showed me my data in context, along with information from my self-monitoring devices (pulse, weight, sleep, and steps per day), as well as notes from online self-evaluations and conversations with a “wellness coach.”
We were a year in, and it was just getting good when they shut down. They cited operational costs, implying that this sort of service is too expensive to provide – at just about any price. I wish I could see the math on that.
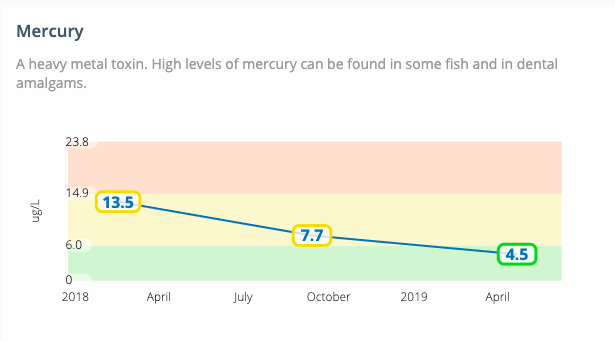
I have written before about my elevated mercury levels and how I was able to do a personal experiment to see whether changing my diet to omit fish rich in heavy metals would reduce them. Here’s a full year plot of the data. It worked.
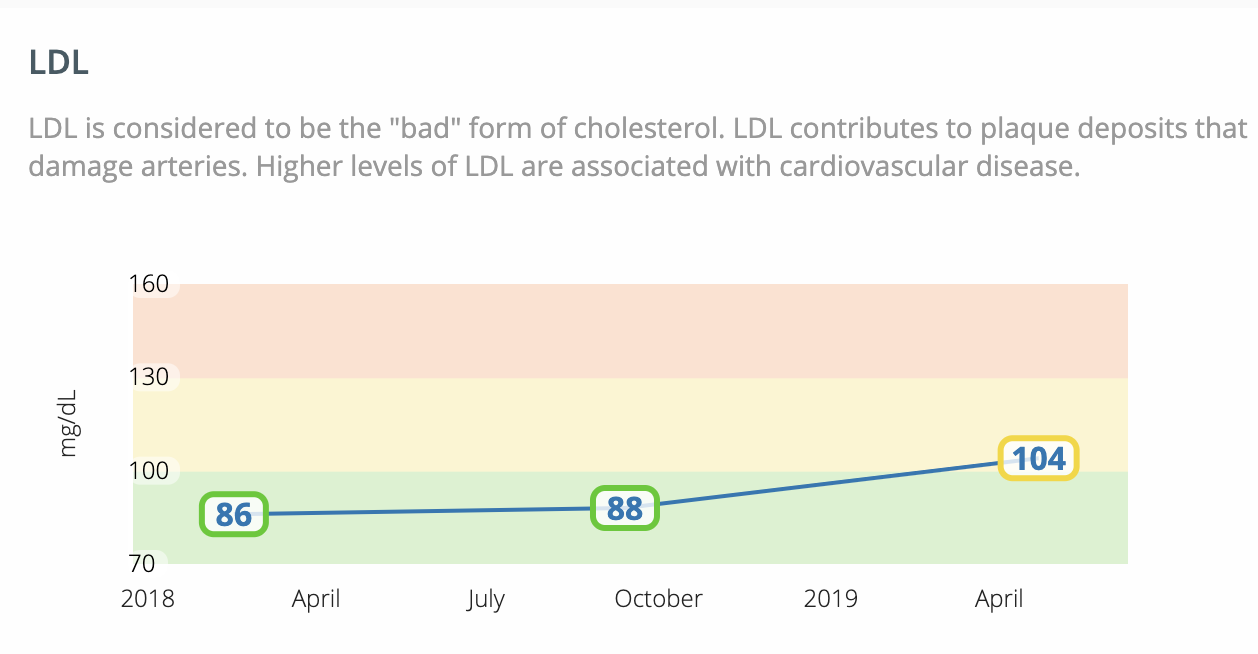
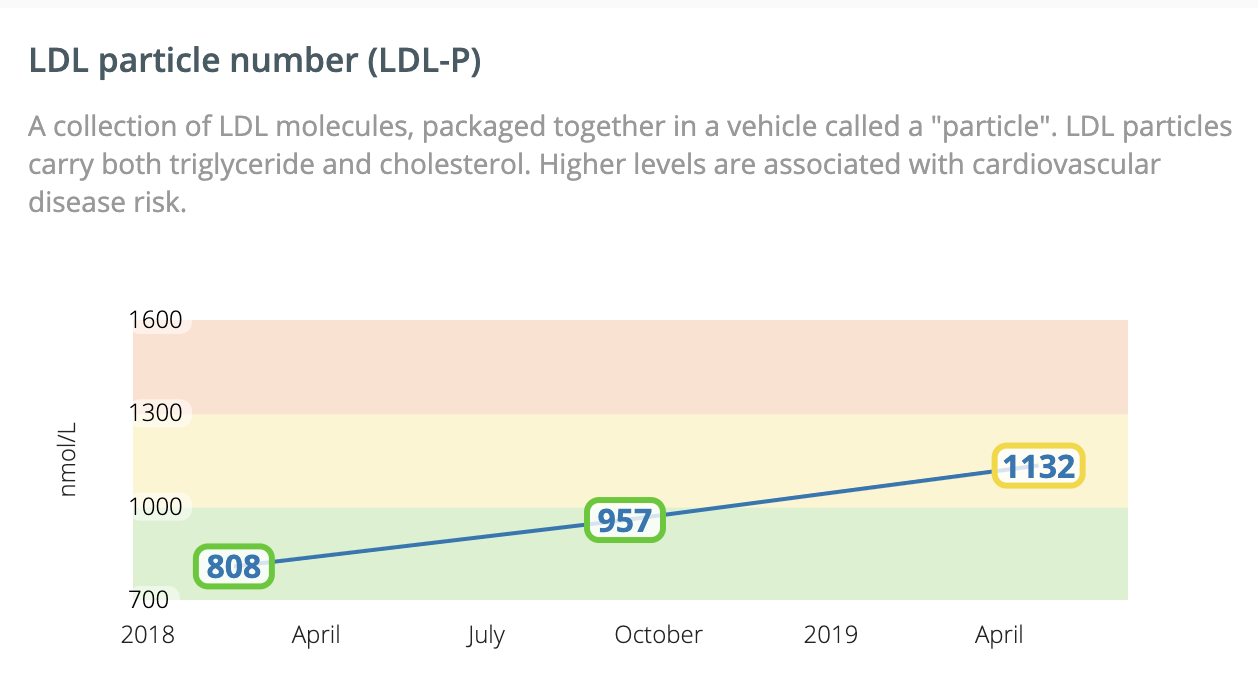
Of course, over the same year, my cholesterol shot up. Here’s a graph of my LDL levels and particle count over the same period:
My first reaction to these plots was to ask “what changed?” One obvious thing that changed was my diet. I had mostly stopped eating mammals and birds around the year 2001. When I cut out mercury rich fish, I re-introduced a bit of red meat. On reflection, I was probably looking to replace the celebration meal-centerpieces that had formerly involved high-on-the-food-chain fish. Also, a slow-cooker roast on a Sunday is pretty wonderful.
The experiment over the next six months will be to dial back down on the red meat and see what happens to the cholesterol. My other grandfather died of heart disease. It’s something I keep an eye on.
Presentation
When I showed these plots to an experienced computational biologist whose PhD includes the word “statistics,” she had a strong reaction. To paraphrase: “What are they thinking, drawing straight lines between those points? That’s incredibly misleading. You got tested three times in a year. Three. This plot gives no insight into the underlying biological variability or the accuracy of the test! This is a gross oversimplification!”
I tried to make a case that the simple picture was accessible enough to spark curiosity and bring a novice like me into a data driven conversation. I told a story about different visualizations that would be suitable for everybody, including patients, data scientists, and also clinicians, all rendered based the same underlying data. She was unimpressed: “It doesn’t matter which of those categories of person we’re talking about, this plot would be misleading to all of them.”
I trust my statistician friend, and I can see the importance of making sure that the data presentation is as accurate as possible. I’m bummed out that I didn’t get to write the feature-request note to Arivale.
The clinic of the future
I will end on a hopeful note: I recently had the opportunity to visit a clinic from the future.
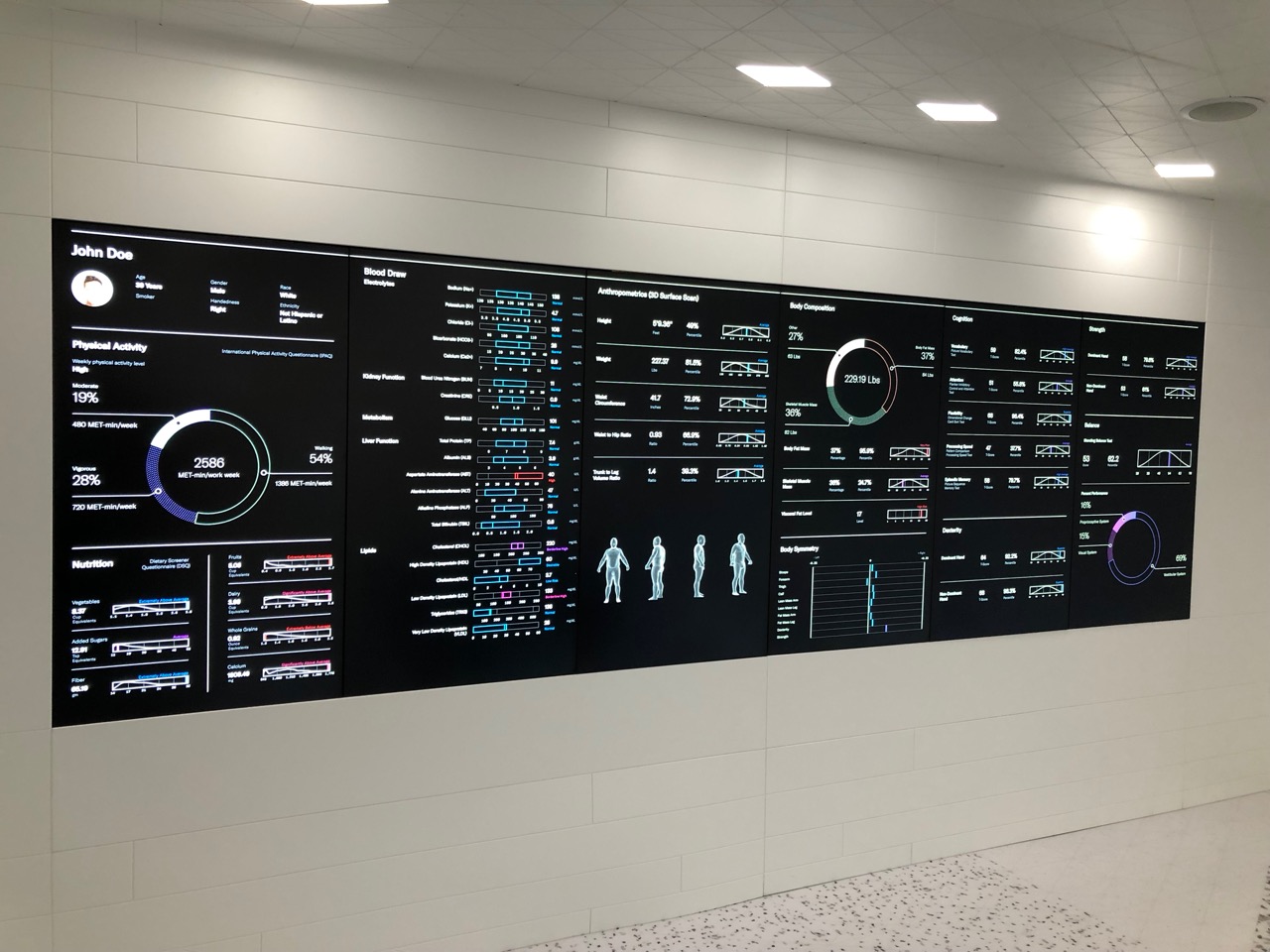
When you walk into Lab100 at the Mt Sinai School of Medicine, it feels more like an Apple store than a medical establishment. Everything is smooth curves, laminate, and frosted glass. Even though the data that they gather is more accurate, better calibrated, and more natively digital (no manual data entry here). The experience is also more personal and human than I’ve previously experienced in a clinical context.
You know how the restaurants and vendors at Disney resorts already know your preferences before you speak up? Imagine that but at the doctor’s office or in the hospital.
A visit to Lab100 begins by sitting down with your caregiver, side by side on a couch. You and the clinician talk while looking at the same pane of glass, a large flat-panel display that shows your medical history and current complaints. Instead of being separated by technology – the flat panel monitor between me and my doctor – here technology brings people together to facilitate that all-important doctor / patient conversation.
The beginning of the visit is a review of your chart to make sure that it’s accurate, complete, and relevant. You move through stations to measure blood chemistry, balance, cognitive function, grip strength, and more. At each station there are video presentations explaining what is being done and why. Your results show up on the screen immediately, including a longitudinal view of how you tested before.
At the end, there is another sofa and an even larger screen where you see yourself in context. Your data is shown along with a cohort of other real people, matched to you by gender and age. Then you and the provider talk and make a plan together.
It’s compelling. I hope that the idea takes off.
It felt like rich people medicine, but the founders of the lab assured me that it is built out of commodity components and designed to be replicated without undue expense. In 2019, the Apple aesthetic is certainly high-end, but for all that, there is an Apple store in every major city in the country. It is apparently possible to have that rich-people feeling while still keeping the coss to shopping mall levels – provided long as you’re selling consumer electronics and not health care.
Lab100 and whoever follows in Arivale’s footsteps are not the whole picture. There is a lot of work still to be done, and many entrenched interests to be appeased. We’ve spent decades building and empire tuned for billing, risk mitigation, compliance, and a weird and stilted flavor of data privacy. It’s going to take years to dig out of this hole.
For all that, the path is clear: Radically empower patients with access and control over their data, and make the physician/patient conversation a 1st class citizen in terms of tool development.
Let’s get on with it.